Pain avoidance:
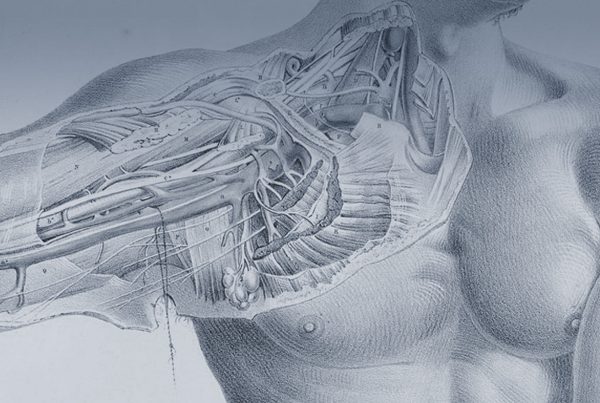
Any nerve when it is cut will try to regrow. The nerve cells (axons) within the nerve will grow out of the cut end looking to find a nerve channel (basement membrane and Schwann cells ideally) to grow down. In a cut nerve, unlike a crushed or stretched nerve) there are no nerve channels for the axons to find so they all wander about looking for one but ultimately giving up. This creates a disorder lump of nerve endings called a neuroma. This lump of nerve endings can be painful due to scarring within in strangling the nerves , or due to the area around the nerve endings being not right (physical of chemical factors being non ideal for the neuroma).
There are many ways to treat the pain from a symptomatic post traumatic neuroma none of which are perfect- So the best way is to try to avoid one forming in the first place. The ways to do this are to provide the nerve cells (axons) with what they want which is a nerve channel (basement membrane and Schwann cells ideally). This can be by if possible reconnecting the nerve with where is would naturally go (restoring anatomic neuronal continuity) or in cases where this is not possible giving the nerve a track to grow into which will stop the neuroma forming. In TMR the track given is a nerve controlling a muscle (a motor nerve).
If the top (proximal) end of a large cut nerve (mixed, sensory or motor) is connected with a motor nerve ending it will grow into it, meaning there is no significant neuroma. It also places the nerve endings in an area where it can be protected from scarring and trauma also making any neuroma that might inadvertently form (from escaped nerve endings) less likely to cause a problem (be ‘symptomatic’).
Natural Movement:
The other use of TMR is to create the environment where the brain can send (transduce) its signals to a robotic device. Image a patient has to have an arm amputated. The nerves that control this arm have to be cut. Usually these are left to grow a neuroma. They are still useful though and send and receive signals to the brain (one reason why they can be painful). Any prosthesis which pics up muscle signals to control the device (myo-electric prosthesis) would usually use the muscles that have not had the nerves to them cut. In an amputation at the level of the arm bone (humerus) this means the biceps and triceps mainly. So control of a prosthetic ‘elbow’ can be naturally triggered via a muscle signal from the biceps, which would when there was an elbow normally bend the elbow. Same with the triceps. If however the prosthesis has a hand that is robotic is has to be triggered by another muscle; one of the muscles of the chest wall, pectorals or latissimus for example. This is not natural, to control grasp or relate by squeezing the arm to the side is possible but not a natural thing to do and has to be learned over time. The nerves that controlled the hand are in the arm still and when the brain thinks to close or open the hand those nerves are getting the signal but they reach a dead end neuroma. TMR allows the natural thought to grasp or release or turn the forearm or extend the wrist and reconnects this to.a muscle. This muscle increases (amplifies) this signal so a sensor (transducer) on this skin can detect it. So with TMR it is possible to control a modern myo-electric prosthesis with ‘natural motor intention’ rather than have to learn new and clumsy controls. It also uses the Neve ends to provide more muscle control points that just leaving them.
It is not yet possible to provide sensation directly to the brain from a prosthesis but at UCL we are researching to provide exactly this for the future.
Timing:
TMR is best undertaken at the same time as amputation but can be done at any point afterwards in most people. There are many ways to design the wiring of a TMR and it is important to coordinate care of the amputation and the prosthetic to get the optimal outcome. I work closely with a number of expert prosthetist and our shared patient benefit from the knowledge of expertise of a professional to guide them through the choices of prosthetic and the journey from planning to delivery.
The team required to deliver maximal outcomes is a large one, it is essential to understand the reasons for amputation, the problems with pain and function likely to be faced post amputation, the functional, analgesic and psychologic rehabilitation necessary is different in every case.
Physiotherapists, Occupational therapists, pain therapists, rehabilitation experts, prosthetists, case mangers, social workers, family, friends it is important to get the right team and the surgeon is only a tiny part of that. I have worked with patients from all walks of life, civilians and military amputees, those with amputations for cancer, infection, trauma and diabetes.